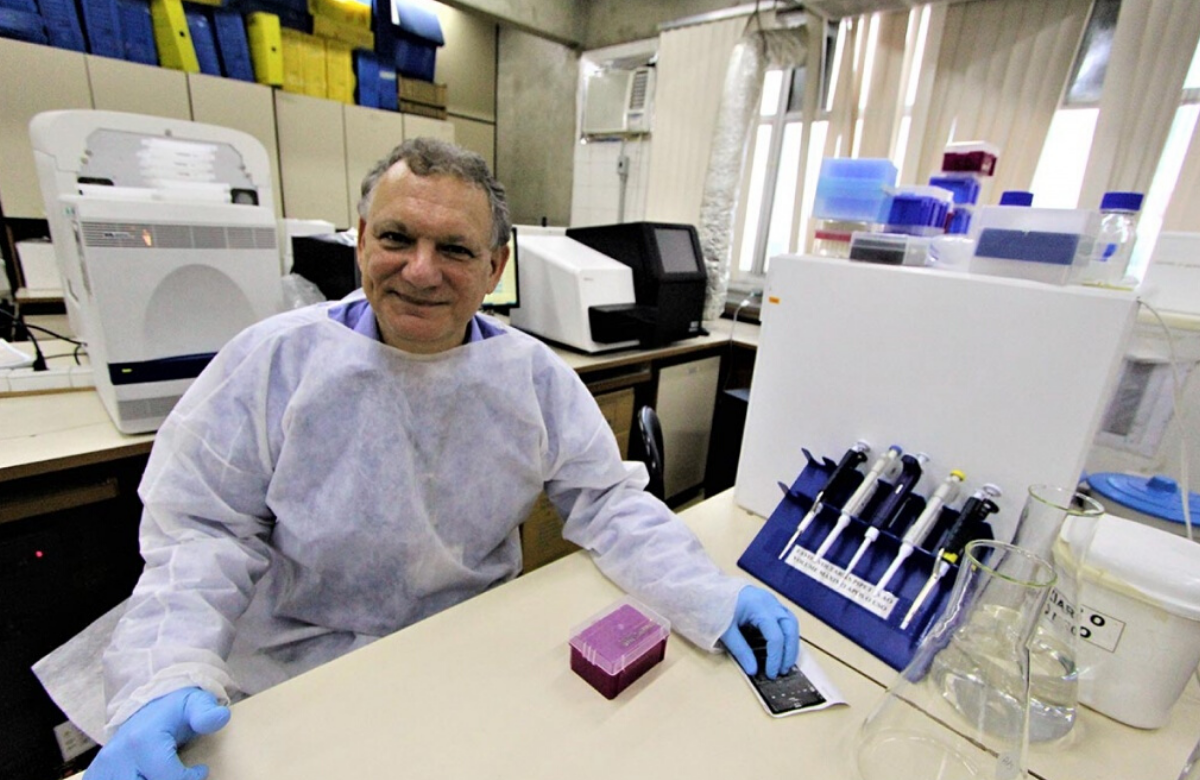
Brazilian man in long-term HIV remission
The findings were presented by lead researcher, Dr Ricardo Diaz, to the 23rd International AIDS Conference (AIDS 2020: Virtual), taking place online this week.
To date, two people appear to have been cured of HIV, Timothy Ray Brown (‘the Berlin patient’) and Adam Castillejo ('the London patient'). Both had cancer and received chemotherapy and transplants with donor stem cells which were largely immune to HIV. But a stem cell transplant is too dangerous for people whose lives are not already threatened by advanced cancer. This has led researchers to ask whether the right combination of medications could offer a safer and less expensive path to long-term remission or a cure.
As part of a clinical trial called SPARC-7, the 35-year-old man in this case added two extra antiretrovirals, the integrase inhibitor dolutegravir (Tivicay) and the entry inhibitor maraviroc (Celsentri), to his existing three-drug regimen. He also received nicotinamide, a water-soluble form of niacin, or vitamin B3. He took this experimental intensified regimen for 48 weeks.
He stopped his antiretroviral therapy under close medical supervision in March 2019. More than 15 months later, he continues to have undetectable HIV RNA (the form of viral genetic material measured in a viral load test) as well as undetectable HIV DNA (the form that largely makes up the viral reservoir).
While this is clearly an interesting case, experts have been quick to caution against reading too much into these results. It involves only a single individual and extensive testing for traces of HIV at various sites in the man's body have not yet been carried out. Four other people treated with the same regimen did not maintain viral suppression.
Injectable PrEP offers superior efficacy to oral PrEP
Headline findings from the study were announced two months ago when it was terminated early because there were clearly fewer infections in people offered injectable PrEP than in people offered oral PrEP. At the time, the researchers could only say that the injectable drug was “non-inferior” to the oral drug.
In his conference presentation, the principal investigator of the study, Dr Raphael Landovitz, was able to say that bi-monthly injections of the drug cabotegravir had passed a predetermined threshold demonstrating superiority, in terms of preventing HIV infection, to oral doses of a combination pill of tenofovir disoproxil fumarate plus emtricitabine (often known by its brand name Truvada).
The study recruited 4566 gay and bisexual men and transgender women, who were randomised to receive either cabotegravir injections plus placebo pills or Truvada pills plus placebo injections. There were 39 infections in people given the pills (1.22% annual incidence) and 13 infections in people given the injections (0.41% incidence). This means there were 66% fewer infections in people given the injections than the pills.
It is not clear whether the infections were the result of poor adherence, as drug concentration and resistance data have not yet been analysed. The most notable side effects were injection site reactions for people receiving cabotegravir injections and decreased creatinine clearance (a measure of kidney function) in a majority of people in both study arms.
A companion study, HPTN084, is underway with 3200 cisgender women in seven countries in sub-Saharan Africa and due to end next year.

How can men be encouraged to take an HIV test?
Previous demographic studies show that men with HIV are consistently less likely to be diagnosed with HIV and less likely to take an HIV test. Understanding the factors that encourage men to test for HIV or make testing more accessible might help to improve testing uptake and HIV diagnosis in men in sub-Saharan Africa.
A team from the large PopART study looked at what factors had encouraged HIV testing during a door-to-door testing campaign in Zambia. They found that testing acceptance was strongly associated with acceptance by other adults (especially men) in the household.
A separate qualitative study from Zambia, exploring health-seeking behaviour among men aged 20-34, found that attitudes to health care and HIV testing were conditioned by fear of stigma and discrimination and of undignified death from AIDS. Men also reported feeling unwelcome in health facilities, being unable to obtain care from male healthcare providers and concerns about having to share facilities with women and children.
In Malawi, researchers looked at men's use of health facilities and HIV testing. It is often thought that men are hard for healthcare workers to reach because they don’t attend health facilities. Although 65% of male respondents had attended a health facility in the previous year and 82% in the previous two years, only 7% said they were offered an HIV test during a visit in the previous year. The lack of testing was most pronounced in men aged 15-24. Many of the men (41%) had attended the health facility as a guardian. Researchers suggested that men could be reached and offered testing during these visits.

Biktarvy in people aged 65 or over
As people with HIV live longer, they are more likely to develop additional health conditions and to be taking multiple medications. However, there are few data on antiretrovirals in people over the age of 65.
Biktarvy, approved in Europe in 2018, is a fixed-dose combination that contains the integrase inhibitor bictegravir, emtricitabine and tenofovir alafenamide (TAF) – a newer formulation of tenofovir that has fewer kidney and bone side effects but may lead to higher lipid levels and weight gain.
The analysis presented to the conference focused on 140 people aged 65 or older who switched from their current antiretroviral regimen to Biktarvy. Nearly 90% of the participants were men, most were white and the median age was 68 years. Many participants had other health conditions, including abnormal blood lipids (59%), hypertension (55%), cardiovascular disease (24%) and diabetes (22%).
At 48 weeks after switching to Biktarvy, 92% maintained viral suppression and none experienced treatment failure. The regimen was generally safe and well tolerated.
Recycling tenofovir better than switch to second-line zidovudine
World Health Organization guidelines recommend the use of tenofovir disoproxil fumarate (TDF) in first-line treatment in resource-limited settings. If first-line treatment fails, the guidelines recommend switching from tenofovir to zidovudine, but twice-daily dosing and the side effects of zidovudine make it an unattractive option.
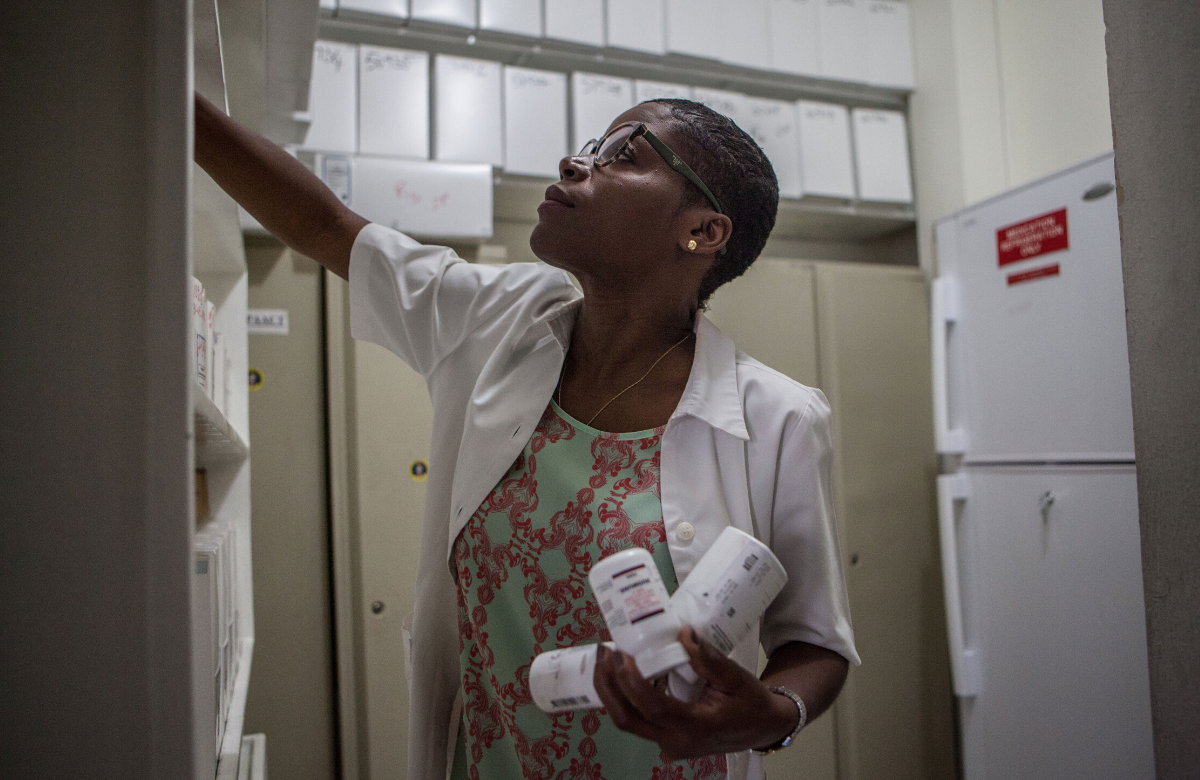
An alternative second-line option is to recycle tenofovir as part of a new combination. Researchers carried out a retrospective review of 1017 adults in Haiti’s GHESKIO HIV clinic who experienced failure of a first-line regimen of tenofovir/lamivudine/efavirenz and who switched to second-line treatment containing either tenofovir or zidovudine, together with a protease inhibitor.
People who continued to take tenofovir were significantly more likely to have a viral load below 200 copies/ml 12 months after changing regimen. They also had significantly better adherence.
Analysis of outcomes according to the protease inhibitor in the new regimen showed that people who continued to take tenofovir and changed to once-daily atazanavir/ritonavir were significantly more likely than people who switched to zidovudine to be retained in care, to have good adherence and to have a viral load test result below 200 copies/ml after 12 months. In contrast, people who continued to take tenofovir but who took it with twice-daily lopinavir/ritonavir were significantly less likely to be retained in care than people who switched to zidovudine and did not have better adherence.
The researchers highlight the important of considering side effects and pill burden when choosing a second-line regimen.

Opportunistic infections in people taking HIV treatment in Latin America
Opportunistic infections are usually seen in people with weakened immune systems who are not taking effective antiretroviral therapy. However, a previous study in Latin America had identified that the median time to diagnosis of cryptococcal meningitis after starting antiretroviral therapy was two years. This surprising finding led researchers to explore the incidence of late-onset opportunistic infections, defined as diagnosis after six months of antiretroviral therapy.
The participants in this study were adults with HIV who started antiretroviral therapy for the first time between 2001 and 2015 in Argentina, Brazil, Chile, Honduras, Peru and Mexico. Of the 8776 participants, 899 had a late-onset opportunistic infection. After five years on treatment, an estimated 8% of people had a late-onset opportunistic infection.
The most common infections were: pulmonary tuberculosis (40%); oesophageal candidiasis (13%); pneumocystis pneumonia (10%); herpes simplex of over one-month duration (7.8%); and disseminated candidiasis (7.3%).
Factors significantly associated with developing late-onset opportunistic infections included female gender, younger age, and lower CD4 count when starting antiretroviral therapy. The researchers recommend closer monitoring for people with these characteristics.

Huge improvements in HIV testing for gay and bisexual men in New South Wales, but some left behind
There has been an “extraordinary scale-up of testing” among gay and bisexual men in New South Wales, Australia since 2010, according to research presented at the conference. Gay and bisexual men make up 80% of all new HIV diagnoses in New South Wales and are a key target group for testing interventions.
As a result of multiple initiatives to increase service capacity and demand, the number of tests being taken increased steadily from 2012 onwards, with an average annual increase of 5.8%. Testing among men at greatest risk increased considerably, from an average of 1.8 tests a year in 2012 to an average of 4.1 tests annually by 2018.
The overall level of undiagnosed HIV in gay and bisexual men fell. However, while undiagnosed HIV among Australian-born gay and bisexual men is currently estimated at under 3%, this success has not translated to other groups. Undiagnosed HIV among overseas-born men appeared to have slightly increased from 15.3% in 2010 to 16.9% in 2018.
Suggested interventions to tackle this disparity include increasing community-based initiatives aimed at overseas-born gay and bisexual men, particularly those promoting self-testing and postal testing. Barriers to accessing PrEP – an issue for black and migrant populations in a number of countries – also need to be addressed.
aidsmapLIVE: AIDS 2020 special

This Thursday 9 July, we are broadcasting an aidsmapLIVE AIDS 2020 special. Joining NAM’s Susan Cole to discuss the biggest stories from the conference are: Dr Laura Waters, Chair of the British HIV Association; Dr Anton Pozniak, President of the International AIDS Society; Professor Linda-Gail Bekker, Deputy Director of the Desmond Tutu HIV Centre; AIDS 2020 plenary speaker Lucy Wanjiku Njenga; and NAM aidsmap’s Gus Cairns.
Join us on Thursday on our Facebook and Twitter pages at 6pm UK time (San Francisco 10am / Rio de Janeiro 2pm / Johannesburg 7pm / New Delhi 10.30pm).
Scientific analysis from Clinical Care Options

Clinical Care Options is the official provider of online scientific analysis for the 2020 International AIDS Conference through capsule summaries, downloadable slides, rapid expert webinars, and ClinicalThought commentaries.
