Abacavir still causing serious cardiovascular problems
Despite guidelines which urge caution over the prescription of the antiretroviral medication abacavir in individuals at higher risk of cardiovascular disease, a large international study has found that 1 in 200 people taking abacavir each year experienced a heart attack, stroke or other serious cardiovascular event. Results were presented to the 18th European AIDS Conference (EACS 2021) yesterday.
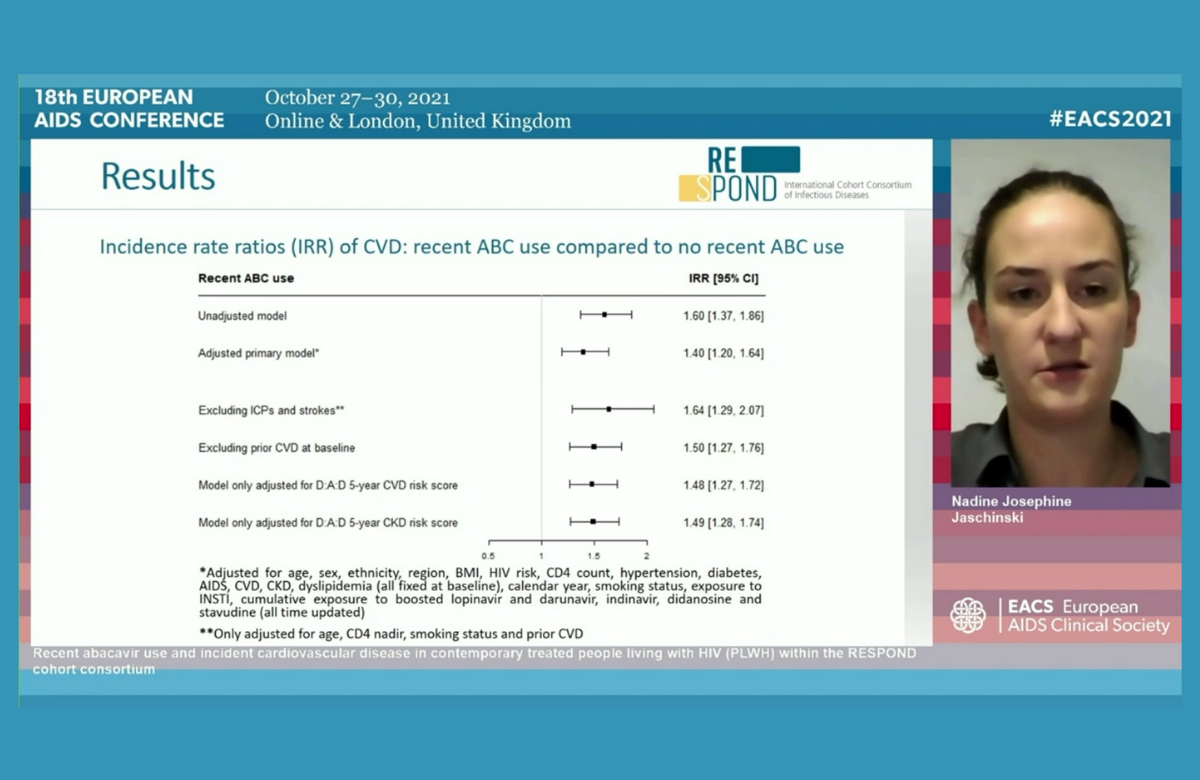
There was no evidence that the risk of a cardiovascular event in people taking abacavir was affected either by predicted five-year cardiovascular risk or chronic kidney disease risk. In other words, people with a lower risk of cardiovascular disease were just as likely to experience an event as people at very high risk.
Data come from all participants in RESPOND, an international collaborative study of 17 cohorts of people with HIV in Europe and Australia. Cardiovascular risk factors were common in this predominantly male, middle-aged group of patients.
While those assessed to be at higher risk of a cardiovascular event were somewhat less likely to be prescribed abacavir, just over a third of participants took the medication at some point between 2012 and 2017, usually with a boosted protease inhibitor.
The investigators calculated the risk of a cardiovascular event in people who had taken abacavir within the past six months compared to people not exposed to the drug. During the study period, 748 cardiovascular events were recorded (299 heart attacks, 228 strokes and 221 invasive cardiovascular procedures) during a median follow-up of 4.4 years. This is a low, but not negligible, incidence of almost 5 cases per 1000 person-years of follow-up, or 1 case for every 200 people taking abacavir each year.
After adjustment for demographic and cardiovascular risk factors, incidence was 40% higher in people recently exposed to abacavir.
First efficacy results from England's PrEP IMPACT Trial
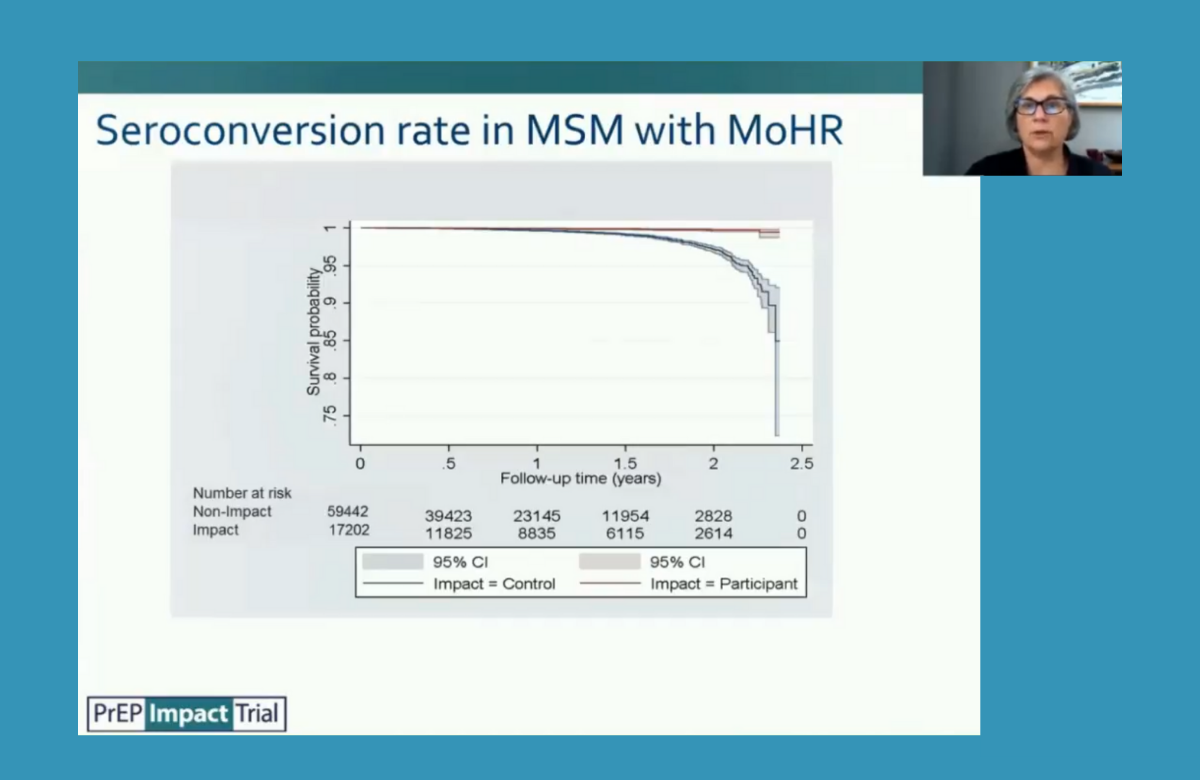
Gay and bisexual men enrolled in the PrEP IMPACT implementation trial in England had 87% fewer HIV infections than a comparable group of sexual health clinic attendees who did not take PrEP, the conference heard.
IMPACT may be the largest PrEP demonstration study ever conducted, with 24,255 participants. Almost 96% were cisgender gay and bisexual men, whom this analysis focuses on.
These participants were compared with cisgender gay and bisexual men attending sexual health clinics who would have been eligible for PrEP on the basis of their sexual risk behaviour.
During the study, 24 male participants were diagnosed with HIV – in all but one case, probably due to non-adherence or having stopped PrEP. The annual incidence rate was 0.13%, whereas it was 1.01% in the comparator group of non-PrEP users.
The researchers tried to use routinely collected data (on sexually transmitted infections (STIs), post-exposure prophylaxis, HIV testing, sex work and known HIV-positive partners) to predict the risk of acquiring HIV, but it turned out that men who did not have these risk factors had a higher incidence than men with markers of higher risk. This was the case for both PrEP users and non-users. This suggests that these markers cannot currently be used to identify sexual health clinic attendees who are most likely to benefit from PrEP.
Data on STIs showed high rates, concentrated in a minority of study participants. While half had no STIs, 26% of men had 80% of the STIs diagnosed in the study.
More screening of domestic abuse needed
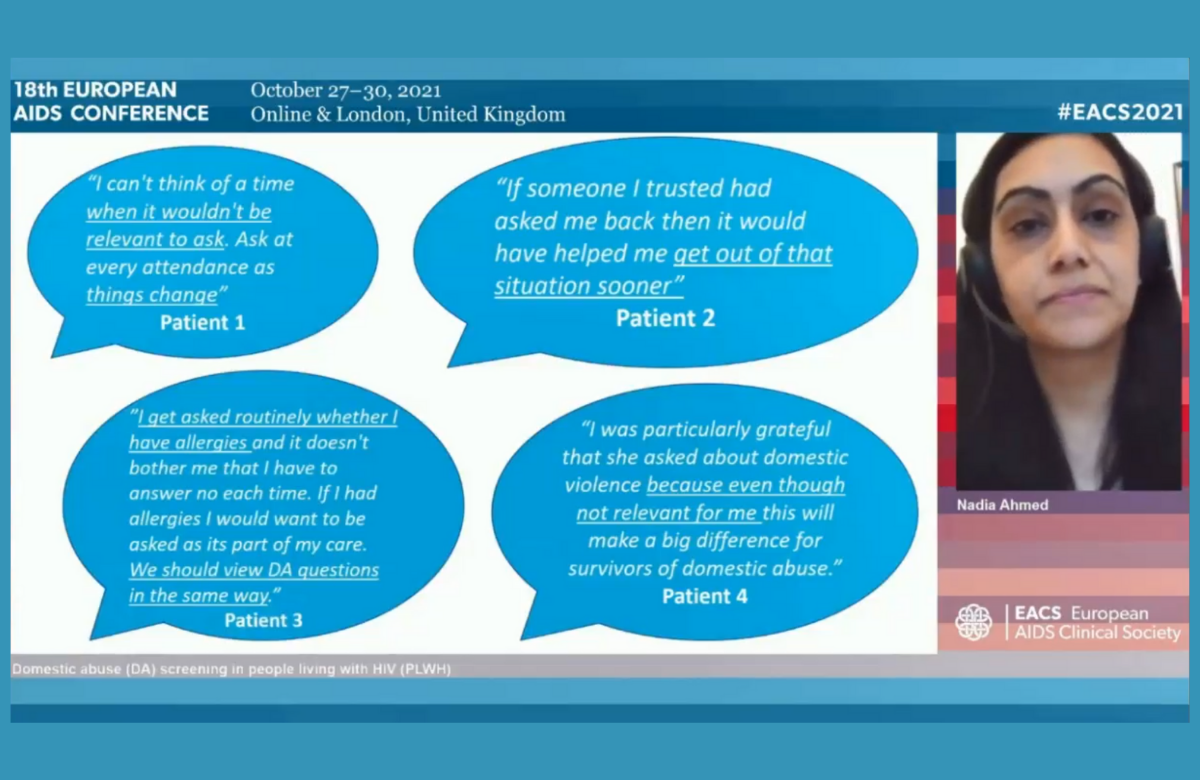
The number of patients at a major London HIV centre who reported domestic abuse tripled after a quality improvement project encouraged staff to routinely ask about it. The majority of disclosures came from non-White British men who have sex with men.
Following staff training, they were sent weekly reminders, including reports of domestic abuse screening rates, with frequent encouragement to ask patients at every visit. Patients who disclosed domestic abuse were referred to health advisors.
The project coincided with COVID-19 lockdowns, which have been associated with increasing cases of domestic abuse.
In the year before the project, physicians screened patients at 8% of visits, rising to 33% between March 2020 and March 2021. The number of patients disclosing abuse increased from 11 to 36. Notably, most patients needed to be asked several times before they felt able to report domestic abuse.
Two-thirds of those reporting abuse were men; a majority of both men and women reporting abuse were not White.
Staff feedback showed increasing confidence in handling the discussion, and patient feedback was positive.
Falling rates of multi-drug resistant HIV
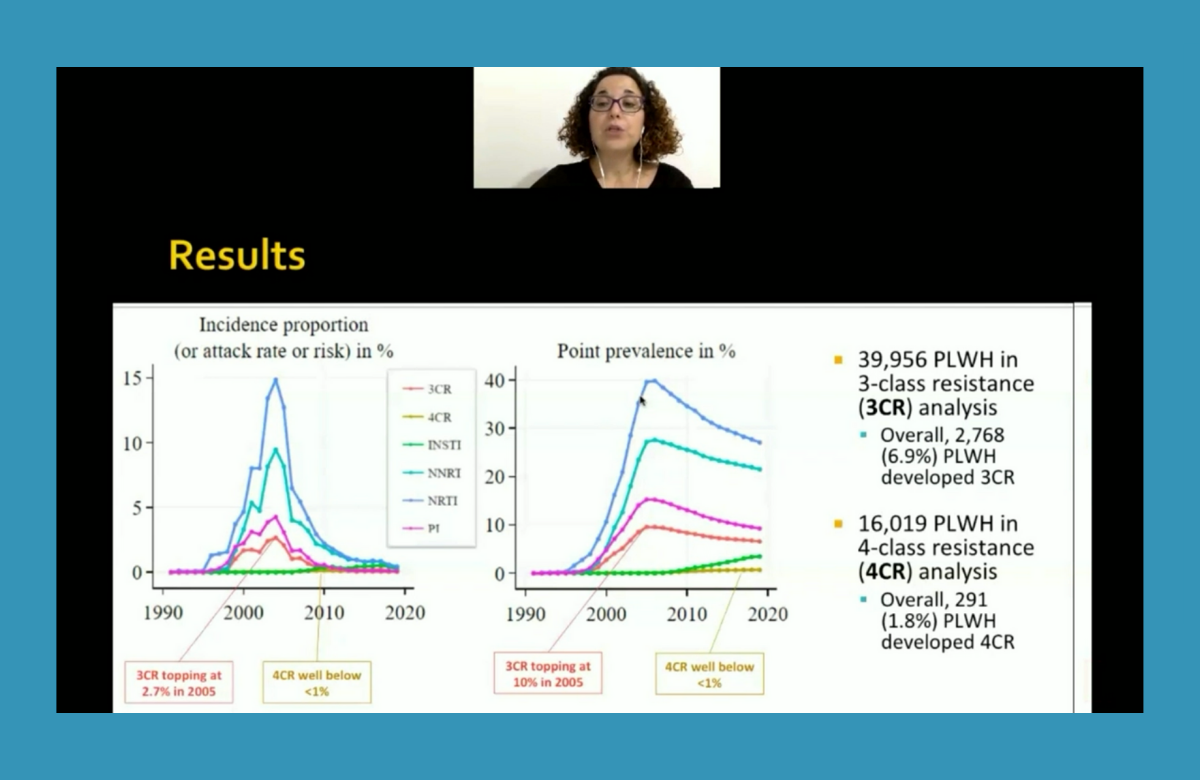
Resistance to all four main classes of antiretrovirals is becoming rarer among people with HIV, data from Belgium, Germany, Italy, Luxembourg, Portugal, Spain and Sweden show.
Notably, the analysis includes data on a broad cohort of people taking antiretroviral treatment, rather than individuals who specifically required resistance testing. The analysis covered almost 40,000 people between 1996 and 2019.
During this time, 6.9% of people on treatment developed three-class resistance. The prevalence of three-class resistance peaked in 2005, when 10% of all people on treatment had three-class resistance. The incidence (rate of new cases each year) of three-class resistance peaked at 2.7% in 2005 and remained below 1% each year after 2010.
Four-class resistance was rare, showing the high barrier of resistance to integrase inhibitors, the newer class of antiretrovirals that was introduced in 2008. A total of 1.8% of people on treatment developed four-class resistance. Prevalence and incidence remained below 1% in all years.
The findings suggest that the development of new antiretrovirals is unlikely to be justified by a need for agents to treat multi-drug resistant HIV.
Speciality guidelines don’t support HIV indicator condition testing
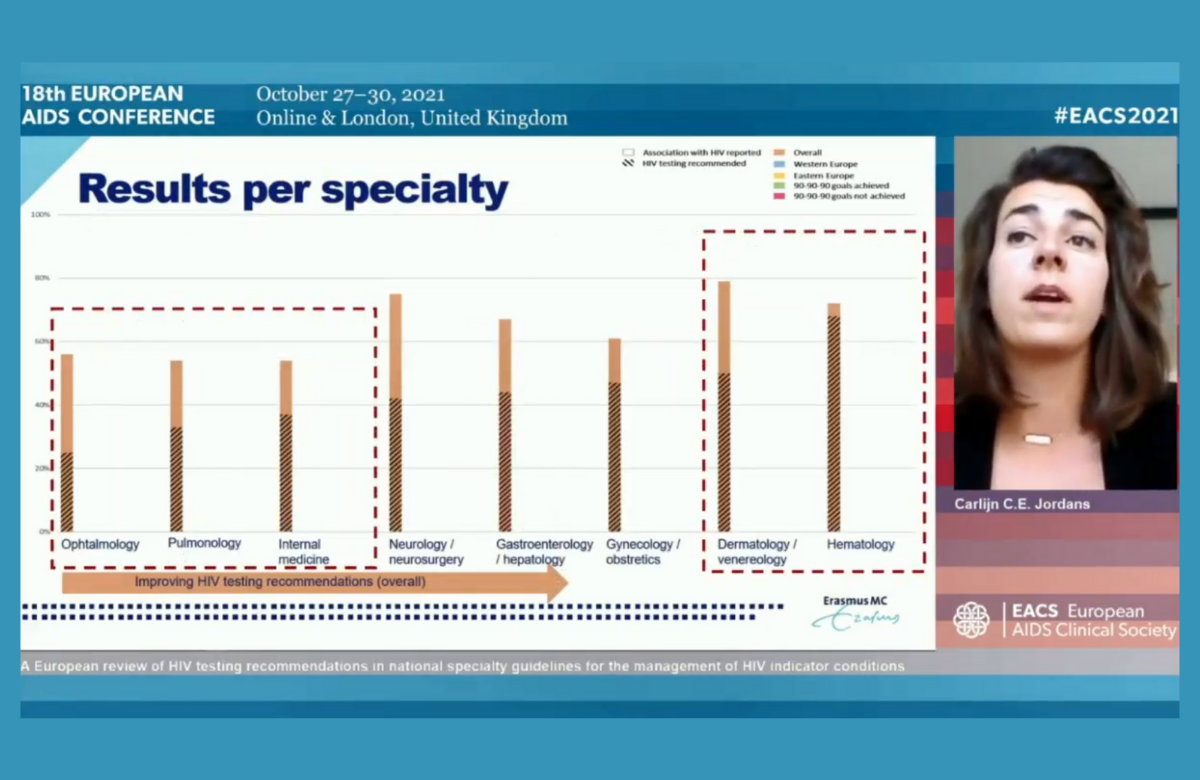
More widespread HIV testing in Europe is being hampered by medical guidelines which do not recommend testing people who have AIDS-defining conditions or other illnesses that could be linked to HIV, the conference heard.
Researchers reviewed 786 national speciality guidelines that cover 63 of these medical conditions – described as ‘indicator conditions’ – in 13 European countries.
Only 65% of guidelines made any mention of HIV testing and only 44% actually recommended it. Even in guidelines covering AIDS-defining conditions, only 50% recommended HIV testing. For example, only 15% of guidelines on cervical cancer and 18% of guidelines on recurrent pneumonia recommended HIV testing.
Guidelines from eastern European countries were more likely to recommend testing than those from western European countries, largely because of better coverage of AIDS-defining conditions.
