There is a dearth of data on transgender and non-binary people receiving HIV care in the UK, but Public Health England (PHE) is beginning to redress this: 123 trans people were recorded as accessing HIV care in England in 2017.
Peter Kirwan of PHE and Michelle Ross of the specialist service CliniQ co-presented the data at the British HIV Association (BHIVA) conference in Bournemouth earlier this month. Whereas PHE’s forms used to ask about gender in binary terms, they have now adopted a two-stage approach that more accurately records diverse gender identities. The first question is, “How do you identify your gender?” and the second, “Is this the same gender you were assigned at birth?”.
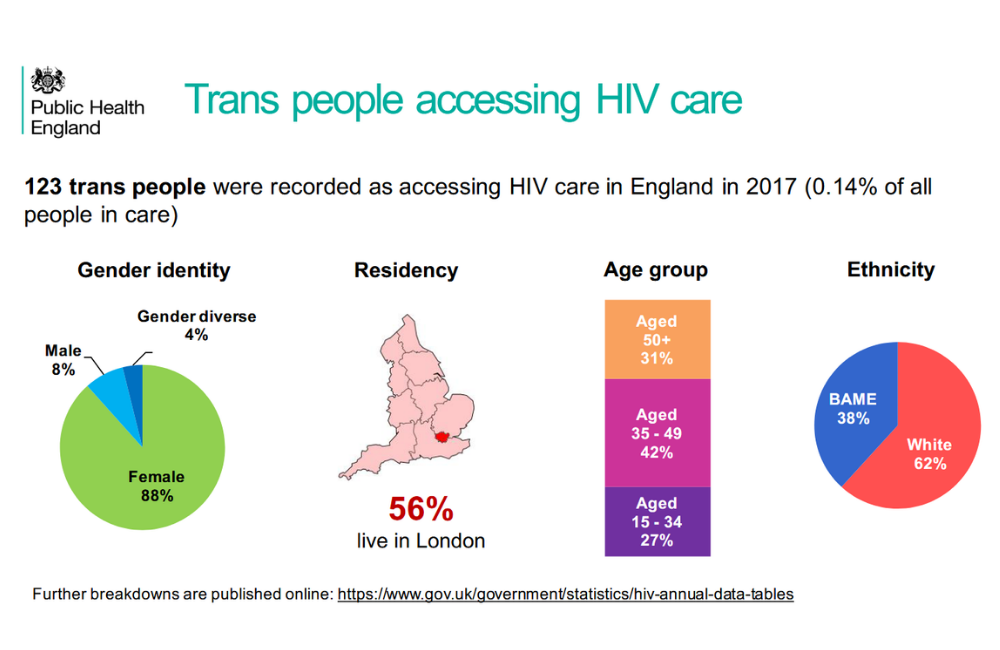
The HIV & AIDS Reporting System (HARS) collects data on each attendance at HIV clinical services. As the new gender questions were only recently introduced, accurate recording of gender identity by clinicians is likely to remain incomplete. Nonetheless, in 2017, a total of 123 individuals were recorded as having a different gender to the one they were assigned at birth (0.14% of all people accessing HIV care).
The vast majority (88%) were trans women, with 8% trans men and 4% identifying in another way. Just over half were living in London, 62% were white and 42% were aged between 35 and 49 years. Figures for the proportions diagnosed late, taking HIV treatment and having an undetectable viral load were the same as for the wider population of people living with HIV. However, the proportion under active psychiatric care (16%) was far higher than for other people living with HIV (4%).
A second data source is Positive Voices, in which a representative sample of 4424 people attending HIV services in England and Wales took part. This was a self-completion survey and a greater proportion of participants identified as trans or non-binary (39 individuals, 0.88%), suggesting that these gender identities were under-reported by clinicians in HARS.
The data from Positive Voices suggests health inequalities – 41% felt depressed or anxious (versus 23% of other participants), 40% said their health was bad or very bad (versus 26%) and 36% reported problems with washing, dressing or other aspects of self-care (versus 13%). In addition, 12% felt they had been refused health care or treatment had been delayed because of their HIV in the past year (versus 7%).
Kirwan P et al. Clinical outcomes and experiences of trans people accessing HIV care in England. British HIV Association conference, abstract O22, April 2019.
Watch the webcast of this presentation.
Update: Following the conference presentation, this study was published in a peer-reviewed journal:
Kirwan P et al. HIV prevalence and HIV clinical outcomes of transgender and gender‐diverse people in England. HIV Medicine, October 2020.
