Key points
- Hepatitis C is a blood-borne infection that is transmitted in some of the same ways as HIV.
- Over time untreated hepatitis C can cause serious liver disease including cirrhosis and liver cancer.
- Modern hepatitis C treatment has few side-effects and can cure almost everyone.
Hepatitis C is an infection that can cause severe liver damage.
Recent estimates find that about 160,000 people in the UK are living with hepatitis C. Overall, about one-third of people with HIV also have hepatitis C, known as co-infection. The majority of people living with hepatitis C do not know they have it. There is no vaccine to prevent hepatitis C.
Over years or decades untreated chronic hepatitis C can cause serious liver disease, and it is one of the leading reasons for liver transplants. Damage to the liver can include:
Fibrosis – build-up of collagen and other fibrous scar tissue, leading to a 'stiff' liver.
Cirrhosis – serious scarring that blocks blood flow through the liver, kills liver cells and interferes with liver function.
Hepatocellular carcinoma (HCC) – a type of cancer that starts in the liver.
End-stage liver disease – severe loss of liver function that can result in death without a liver transplant.
Treatment of hepatitis C has improved rapidly in recent years. Modern treatment typically lasts for two or three months, usually does not cause side-effects and cures more than 95% of treated people. For information on treatment of hepatitis C, see our treatment page.
Transmission and prevention
Hepatitis C transmission happens in some of the same ways as HIV transmission. It is usually passed on by direct blood-to-blood contact. In the past, many people acquired hepatitis C from blood products given during medical procedures – for example blood transfusion during surgery or treatment for haemophilia – before blood screening and sterilisation were introduced in the UK in 1991.
Today, the most common route of transmission in the UK is sharing needles and other equipment for injecting drugs or anabolic steroids. To reduce the risk of transmission or reinfection:
- Avoid sharing injecting equipment (needles and syringes).
- Avoid sharing drug preparation equipment such as spoons, filters, water, water containers. Tiny amounts of blood from someone who has previously used the equipment may be present.
- Avoid sharing bank notes or other items for snorting drugs. Tiny amounts of blood from someone who has previously used them may be present.
Sexual transmission of hepatitis C is less common, but it does occur. Since around 2000, there has been an increase in the number of gay and bisexual men living with HIV who have acquired hepatitis C through sexual transmission in the UK and elsewhere. However, sexual transmission of hepatitis C to HIV-negative gay men and between heterosexual people appears to be uncommon.
Sexual transmission of hepatitis C has been linked to several factors including anal sex, rough sex, fisting, group sex, having other sexually transmitted infections, sharing sex toys and using non-injected recreational drugs during sex. Hepatitis C can be transmitted when blood is present during sex, but hepatitis C can also sometimes be found in semen and rectal secretions.
Condoms can reduce the risk of sexual transmission of hepatitis C as well as HIV, hepatitis B and other sexually transmitted infections. Using gloves for fisting may also help prevent hepatitis C transmission. To reduce transmission risk in group sex situations, don’t share sex toys or pots of lubricant. Change condoms and gloves between partners. Clean any hard surfaces, such as benches or slings, between uses.
Some gay men living with HIV try to only have unprotected sex with other men who are also living with HIV (often called ‘serosorting’). However, this does not protect against hepatitis C, hepatitis B or other sexually transmitted infections. HIV pre-exposure prophylaxis (PrEP) also offers no protection against hepatitis C.
Mother-to-child transmission of hepatitis C is uncommon, but the risk is higher if the mother is living with HIV as well as hepatitis C. Having a high hepatitis C viral load increases the likelihood that hepatitis C will be passed on.
It is also possible to acquire hepatitis C through personal care items such as razors, toothbrushes and manicure tools that may come into contact with blood. These items should not be shared. New, sterile needles should be used for piercings, tattooing and acupuncture.
Hepatitis C is not transmitted through normal social contact such as sharing crockery or cutlery, or touching someone with hepatitis C. Blood spills from someone with hepatitis C should be cleaned up following sensible infection control procedures (e.g. wearing gloves and using appropriate cleaning products). Scratches, cuts and wounds should be cleaned with soap and water and covered with a waterproof dressing or plaster.
There is currently no vaccine to protect against hepatitis C. Unlike hepatitis A and B, having hepatitis C once does not mean you are immune. If you naturally cleared hepatitis C or have completed successful treatment, you can be re-infected if you are exposed to hepatitis C again.
Diagnosis and monitoring
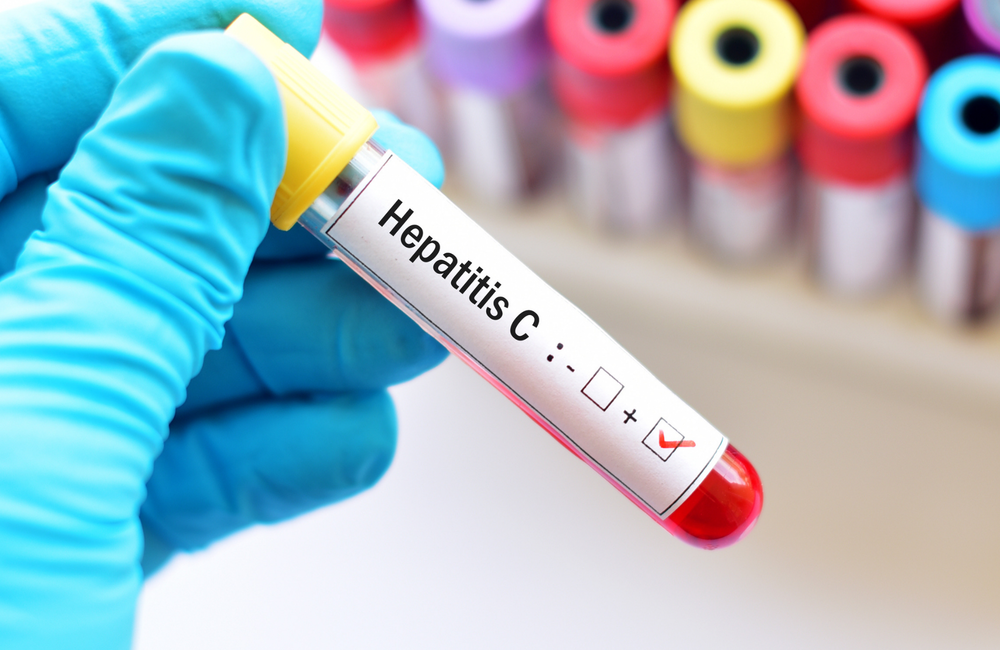
If you are at risk, it makes good sense to be tested regularly for hepatitis C. Knowing you have hepatitis C will allow you to have the health of your liver monitored. Hepatitis C treatment has the best chance of success if it is started soon after infection.
Current guidelines say that all people with HIV should be screened for hepatitis C at the time of HIV diagnosis and then at least once a year thereafter. If you share injecting equipment, use drugs during sex (chemsex), have a new sexually transmitted infection, or have sex that involves contact with blood, fisting or sharing of sex toys, more frequent testing will allow recent infection to be detected sooner. This will allow you to begin treatment during the early phase of infection and will also limit the chance that hepatitis C is passed on to anyone else. A blood test can show if you have been exposed to hepatitis C and have produced antibodies against it. Another type of test measures hepatitis C viral load or presence of hepatitis C virus genetic material (also known as HCV RNA) in the blood. Detectable viral load means the virus is actively replicating in your body.
A positive hepatitis C virus antibody test should be followed by a viral load test and a test to determine the hepatitis C genotype. Viral load and genotype are two factors that affect treatment outcome.
"Hepatitis C can be transitted when blood is present during sex, but hepatitis C can also sometimes be found in semen and rectal secretions."
If you may have been exposed to hepatitis C and you have unexplained abnormal liver function tests, you should have an HCV RNA test to see if you have recent, or acute, infection and are in the period before hepatitis C antibodies have been produced.
If you are diagnosed with hepatitis C you should have regular liver function tests to see how well your liver is working. A liver function test is also recommended when you are first diagnosed with HIV, at each routine HIV clinic appointments and if you become ill.
Liver function tests include two enzymes, known as ALT and AST, which can indicate liver inflammation. High levels of these enzymes can mean you have hepatitis C or antiretroviral drugs are harming your liver. However, some people with hepatitis C still have normal liver function tests despite significant liver damage.
Other types of tests are done to see how much the liver is damaged, which indicates the urgency of treatment. One test, called elastography (FibroScan), uses vibration waves to determine the degree of liver fibrosis or cirrhosis. Another is a liver biopsy, which uses a hollow needle to remove a small sample of liver tissue to examine under a microscope. Doctors also use a number of blood tests that can indicate the health of your liver.
People with chronic hepatitis C who have advanced fibrosis or cirrhosis should be screened every six months for liver cancer, which is usually done with ultrasound scans.
Symptoms and disease progression
The majority of people do not experience symptoms when they first acquire hepatitis C, a period known as acute infection. Among people living with HIV, routine liver function tests sometimes reveal elevated liver enzymes that can be a sign of liver inflammation due to hepatitis C.
When they do occur, signs and symptoms of acute hepatitis C infection may include the following:
- fatigue (unusual tiredness)
- fever
- nausea and vomiting
- pain in the upper abdomen or belly
- feeling generally unwell (malaise)
- yellowing of the skin and whites of the eyes (jaundice).
Around 10 to 25% of people who acquire hepatitis C will clear the virus without treatment. Most people develop chronic hepatitis C that lasts more than six months. People living with HIV appear less likely to spontaneously clear hepatitis C. People with chronic infection will continue to be infectious and can pass on the virus to others, whether or not they have symptoms.
Over the longer term, about half of people with chronic hepatitis C will experience some symptoms. The most common include fatigue, loss of appetite, muscle and joint pain, and feeling generally unwell. Some people may experience 'brain fog' (mild cognitive problems) or depression. Symptoms may worsen or become more numerous over time.
These symptoms can have a negative impact on work, family life, social life and sex life. If this is the case for you, be sure to tell your doctor about the problems the symptoms cause you.
Chronic hepatitis C can contribute to conditions beyond the liver, known as extra-hepatic conditions. Studies have found that people with hepatitis C have a higher risk for joint and skin problems (cryoglobulinaemia), heart disease, strokes and diabetes. Research increasingly shows that infection with HIV, hepatitis C or both contributes to chronic inflammation, which can lead to problems throughout the body.
Over years or decades, chronic hepatitis C can cause serious liver damage including fibrosis, cirrhosis and liver cancer. Some people never experience any of these complications. But up to 20% of people with hepatitis C will develop cirrhosis, usually over two or three decades. People with HIV have faster liver disease progression, on average. In the most severe cases, hepatitis C can lead to liver failure, the need for a liver transplant or liver-related death.
Hepatitis C and HIV
About 10% of people living with HIV in the UK also have hepatitis C, known as co-infection. This is much more common in certain groups, such as people who inject drugs.
HIV co-infection affects hepatitis C, but having hepatitis C does not seem to make HIV disease worse. People living with HIV are less likely to naturally clear hepatitis C. They also tend to have more aggressive liver disease progression, particularly if they have a low CD4 cell count. Research done in the era of effective and well-tolerated antiretroviral therapy finds that people with well-controlled HIV can do nearly as well as HIV-negative people.
People living with HIV do not respond as well to the old interferon-based therapy for hepatitis C, but this is not the case with the new direct-acting antivirals. People living with HIV and hepatitis C co-infection can be treated with most of the same hepatitis C regimens as HIV-negative people and their cure rates are the same.
Reinfection after treatment
Some people may become reinfected with hepatitis C after being cured. Some studies show quite a high rate of reinfection in gay and bisexual men. There is no evidence that people who are cured of hepatitis C are protected against future reinfection, so it is important to take precautions to avoid reinfection. Speak to your healthcare team if you think that you need help to avoid reinfection, such as treatment to reduce or stop injecting drugs, access to clean injecting equipment or psychological support to reduce risk-taking behaviour.
Living with hepatitis C: your lifestyle
People living with HIV and hepatitis C can benefit from adopting a healthy lifestyle, including eating a balanced diet. Try to maintain a healthy weight. Being overweight is linked to fatty liver disease, which can worsen liver damage.
Since people living with HIV and hepatitis may have an increased risk of cardiovascular disease and diabetes, your clinic should regularly monitor your blood fats or lipids (cholesterol and triglycerides) and blood sugar (glucose).
People living with hepatitis C should limit how much alcohol they drink, and those with liver damage should avoid alcohol altogether. Not smoking and cutting down or stopping recreational drug use are also important for overall health.
- Eat a balanced diet including vegetables, fruit and wholegrains.
- Get regular moderate exercise.
- Stop smoking.
- Reduce or eliminate alcohol and drug use.
- Get enough sleep.
- Find ways to reduce stress.
Other sources of information
For more information, you may find these two organisations helpful:
- Hepatitis C Trust: www.hepctrust.org.uk. You can contact their helpline team on 020 7089 6221.
- British Liver Trust: www.britishlivertrust.org.uk. You can contact their helpline team on 0800 652 7330.